“Care management programs apply systems, science, incentives and information to improve medical practice and assist consumers and their support system to become engaged in a collaborative process designed to manage medical/social/ mental health conditions more effectively.” (Center for Health Care Strategies, 2007)
Care Managers employed by Jackson Health Network are either a Licensed Master Social Worker (LMSW) or Registered Nurse (RN) who are experts in managing complex medical conditions, motivational interviewing, care coordination and all stages of change a patient may experience. Care managers have proven to be a vital component of the care team and have successfully been embedded into primary care.
All primary care clinics have a fully integrated care manager at their practice. Primary care offices have the option of contracting with JHN to access its shared care management team or hiring their own qualified care manager. Since the inception of this care team model in 2017, there has been a significant improvement in provider satisfaction.
Care managers work in collaboration with contracted Community Navigation Specialists to address the socio-economic needs of patients. Community Navigation Specialists provide clerical, task-based work associated with Care Management, and Transition Coordination services are contracted by JHN through the Central Michigan 2-1-1 program. These individuals primarily focus on linking patients to services in the community, including access to housing and food, assistance with medication co-pays, and transportation to and from doctor appointments. In addition to their work with care management, these individuals are experts at connecting patients to resources in the community, using both their in-depth database and the Jackson Care Hub.
The Jackson Care Hub was designed as a result of the Clinical Community Linkages strategy. The Hub is an online platform that allows community organizations to screen for SDOH and assess an individual’s needs in order to determine the most appropriate resources. An electronic referral to the selected organization can then be made in real time. The system also allows the receiving organization to manage the referral and work it through to completion. As the organization manages the referral, the original screening organization is provided with real time feedback of the progress being made.
The highest areas of need in our community have been identified through data collection efforts. The table below shows a breakdown of positive SDOH needs identified by domain. The data is used to inform existing and new services and resources offered in the community and ensures the needs of the community are met.
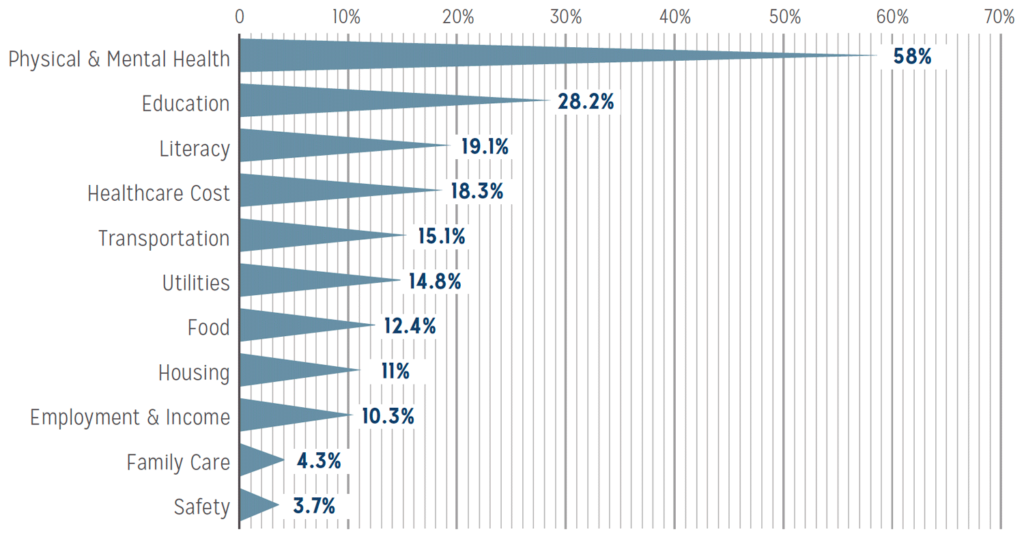
Source: Jackson Care Hub Data Brief 2/2020-7/2020